Lyme Disease: More Than a Rash
- Carrie Ballas

- May 26, 2025
- 4 min read
If you’ve ever lived in or traveled to areas like the East Coast, the Upper Midwest, or other tick-endemic regions, it’s crucial to understand the long-term risks of Lyme disease and its many co-infections. Even years later, symptoms can emerge that often go unrecognized or misdiagnosed by traditional medicine.

While the most well-known culprit causing Lyme disease is a tick-borne disease caused by the Borrelia bacteria, 27 other tick-borne pathogens have been identified globally, and at least 18 are found in the United States. Some of the most common and well-known pathogens that cause Lyme disease include:
Bartonella
Babesia microti
Babesia duncani
Babesia species (California type)
Ehrlichia ewingii
Ehrlichia chaffeensis
Ehrlichia muris eauclairensis
Rickettsia rickettsia (Rocky Mountain Spotted Fever, rare in Colorado)
Rickettsia philipii
Borrelia miyamotoi
Borrelia mayonii
Borrelia spp. (others in Europe and the USA)
Anaplasma phagocytophilum
Mycoplasma spp.
Chlamydia spp.
Brucella
Tularemia
Powassan virus
Heartland virus
Bourbon virus

It’s important to note that not all ticks carry these pathogens, but they can also carry co-infections with multiple pathogens. Clinicians should be aware of both the Borrelia species and these other co-infections when considering Lyme disease. Co-infections behave differently, which is one reason why a single course of Doxycycline is often insufficient for many patients to recover fully.
Most Lyme patients never recall a tick bite, and it has been estimated that up to 50% will not present with a rash (bull’s-eye rash), but that doesn’t mean they’re in the clear.
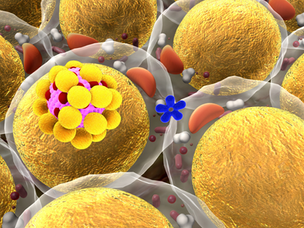
It is also important to note that some infections, like Bartonella, can be transmitted by other vectors such as, fleas, flies, mites, or spiders, and they hide inside cells, making them particularly difficult to detect and treat.

Early Lyme Disease: Recognizing Initial Symptoms
Symptoms that can occur within the first few days or weeks after infection can include:
Fever and chills
Headache
Fatigue
Muscle and joint aches
Swollen lymph nodes
Neck stiffness
Chronic Lyme and Co-Infections: The Hidden Epidemic
Lyme disease can persist, especially when left untreated or under-treated. Chronic Lyme, or Post-Treatment Lyme Disease Syndrome (PTLDS), is still not fully recognized in conventional medicine, but it affects countless individuals. Symptoms may appear weeks, months, or even years later and include:
Dizziness
Sleep disturbances
Facial palsy
Light Sensitivity
Nerve pain, numbness, or tingling
Brain fog and cognitive impairment
Psychiatric symptoms such as Depression and Anxiety
Irregular heartbeats, arrhythmias, and chest pain
Shortness of Breath “air hunger”
Rashes, including stretch marks
Arthritis and migratory joint pain
Chronic pain
Neck stiffness
Fatigue
Headache and Migraines
Testing Limitations: Why Many Cases Are Missed
Standard Lyme tests, including ELISA and Western blot, are commonly used but flawed. Studies show they can miss up to 50% of cases, especially in early stages or chronic presentations. That’s why we often recommend more advanced testing through specialty labs such as:
IGeneX
AcuDart
Vibrant Wellness
Tlab
Galaxy Diagnostics
ArminLabs
These labs can help identify Borrelia and co-infections with more accuracy. Methods include direct microscopy, highly sensitive diagnostics, the use of recombinant technology in antibody testing, and testing using DNA “PCR” analysis. These companies test and target multiple species, which can increase the detection rate considerably and reduce false-negative results.
What Should You Do If You Suspect Lyme or Mold?
If you have persistent and unexplained symptoms, and especially if you’ve been in tick-endemic areas, a helpful first step before exploring further testing or treatment is to take the free online MSIDS questionnaire, developed by Lyme specialist Dr. Richard Horowitz, MD. This questionnaire helps determine the probability of you having MSIDS, Lyme disease, and /or other tick-borne illnesses.
How We Support You at Boulder Integrative Health
At Boulder Integrative Health, we take a whole-body, root-cause approach to Lyme and chronic infections. Although I (Carrie) don’t label myself as a Lyme Disease Specialist, who often only focuses on Lyme Disease (some people need these providers specifically), I do work with patients with Lyme disease using a whole-body approach. These are some ways I get my patients to restore their wellness.
Addressing any mold toxins that may be impacting the immune system and making it challenging to heal from Lyme.
Nervous system retraining (e.g., DNRS)
Herbal antimicrobials and targeted nutrients (antibiotics when needed)
Gut microbiome restoration
Mitochondrial and detox pathway optimization
IV therapy tailored for chronic infections
Sauna therapy, lymphatic drainage, and binders
Lifestyle support: restorative sleep, yoga, movement, meditation

Genetics and Inflammation: What You Should Know
Up to 25% of people have HLA-DR/DQ genetic variants that impair their ability to clear biotoxins. These individuals are more prone to Chronic Inflammatory Response Syndrome (CIRS), a complex condition triggered by Lyme Disease, Mycotoxins, Dinoflagellate toxins, Actinomyces, COVID-19 virus, Epstein-Barr Virus, and other biotoxins.
You’re Not Alone... Let’s Figure It Out Together
While I am not a dedicated Lyme-only specialist, I have supported many patients through diagnosis and recovery, and I can also refer you to top Lyme-literate practitioners when appropriate. My IV clinic, IV Boulder, also offers supportive therapies for chronic infections. If your symptoms align with Lyme disease, please reach out. You don’t need to navigate this alone.
In health and wellness,
Carrie Ballas
Boulder Integrative Health
Resources
AcuDart has a discount for Lyme Disease Awareness Month (offer ends 5.31.2025)