How is your colon doing, and how do you really know
- Carrie Ballas

- Mar 13, 2023
- 11 min read
Updated: Jan 4, 2025

Did you know the screening for Colon Screening now starts at age 45?
Why so early do you say?
Colorectal Cancer (CRC) has increased significantly in the United States, and nearly 18,000 people under the age of 50 will be diagnosed with CRC in a year. The determination by the U.S. Preventative Services Task Force is to recommend regular screening as a key way to preventing CRC, which can save lives when found early.
Screening for CRC is recommended for people with an average risk for disease from age 45 to 75, and thereafter is based on an individual basis.

STATS
In the U.S. Colorectal Cancer is the 3rd leading cause of cancer related deaths in women and men
The overall lifetime risk of developing CRC is 1 in 23 for men and 1 in 25 for women
There are 106,180 new cases of colon cancer per year
There are 44,850 new cases of rectal cancer per year
70% of people diagnosed with CRC have no family history of the disease
Colorectal cancer and how it develops Polyps
Cancer starts as a growth on the inner lining of the colon or rectum called a “polyp”. Polyps are asymptomatic and benign initially, meaning they are not cancer, but certain types and shapes of polyps can develop into cancer over time. Cancerous polyps start in the innermost layer (mucosa) and grow outward and into blood vessels, lymphatic vessels and distant parts of the body, which then means it has metastasized.
Polyps are considered either Neoplastic or Nonneoplastic
Neoplastic polyps “a neoplasm is when cells form into a mass or tumor”. Neoplasms can be benign, pre-cancerous or malignant, however neoplastic polyps, such as adenomas and sessile serrated polyps do have a risk of developing into cancer and are therefore removed.
Nonneoplastic polyps rarely turn into cancer, which include hyperplastic polyps, inflammatory polyps and hamartomatous polyps. These polyps will still sometimes be removed and biopsied in cases of uncertain identity during examination.
I will now describe the shapes noted on pathology reports and the types of polyps that are identified, so that you will have a better understanding when you get your report after a Colonoscopy screening. There are three main polyp shapes:
Stalk or mushroom-like (pedunculated) Flat (sessile) Saw-toothed (serrated)
The pedunculated polyps are easy to see and remove. Sessile polyps are harder to see because they are flat and are often missed during examinations. Serrated polyps can also be missed if they are located further up the colon and are often missed during examinations.

Five types of Polyps:
Adenomatous polyps (pedunculated): A neoplastic polyp that is considered pre-cancerous, and over time can turn into cancer. About 70% of polyps founds are of this type and these are always removed, biopsied and require closer monitoring as a result.
Sessile Serrated polyps: A neoplastic polyp that is also considered “pre-cancerous” depending on size. Larger sessile serrated polyps are flat and if located in the upper colon they are difficult to detect and can be missed and therefore can turn into cancer. The larger the polyp the greater the risk of cancer. Most colorectal cancers are adenocarcinomas.
Hyperplastic polyps: (serrated): A nonneoplastic polyp is relatively common and tends to develop in parts of the digestive tract where tissues have been previously damaged. They are usually small at the lower end of the colon and have very little potential to become malignant.
Inflammatory polyps: A nonneoplastic polyp arises in tissues damaged by chronic inflammation such as IBS, Crohn’s disease and Ulcerative colitis and have very little potential to become malignant.
Hamartomatous polyps: A nonneoplastic polyp that is considered to be related to an inherited genetic condition. Although the polyps themselves aren’t considered cancerous, the genetically vulnerable cells can divide abnormally and can lead to cancer.
Anal Cancer
I would be remiss not to mention anal cancer. Anal cancer only accounts for 2.5% of digestive cancers, however rates are increasing. 90% of Anal cancers are associated with the human papillomavirus (HPV), specifically type 16 and 18. There can be precancerous cells in the anus and they are called “dysplastic cells” and if they become severe, this increases risk of anal cancer.
Symptoms
Often asymptomatic
Growth in or around the anus
Itching
Bleeding
Screening for Anal cancer
Screening starts with a digital rectal exam, but to assess cells for dysplasia, one needs an anal Pap Test and then a biopsy. Unfortunately screening for anal cancer is not recommended for the general population so finding a clinician trained in anal pap exams would be recommended, especially if you are at risk or have symptoms.
So who is at the highest risk for colorectal cancer?
Family history of colorectal cancer or colorectal polyps
Personal history of Inflammatory Bowel Disease, Crohn’s Disease or Ulcerative Colitis
Certain ethnic groups are at a greater risk, such as Alaska Native, American Indian, Ashkenazi Jews, Black people and White people.
Causes and risk factors for colorectal cancer
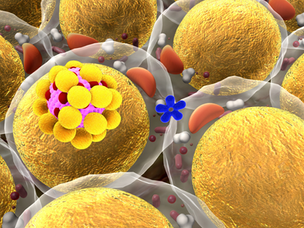
Obesity (fat causes pro-inflammatory cells that contribute to the growth of cancer)
High Insulin and uncontrolled Diabetes (insulin is an inflammatory hormone that encourages cancer to grow)
Inflammation in the body
Smoking
Chronic constipation
Lack of exercise and sedentary lifestyle (exercise improves stool transit time and it overall reduces inflammation)
Excessive alcohol (alcohol is converted into acetaldehyde, a potent carcinogen, which can reduce the body’s ability to repair damaged DNA and defend against free radicals)
Toxic Chemicals
Abnormalities in the gut microbiome
Unhealthy diet (meaning high in refined sugars, trans fats, standard red meat, processed meats, eating low anti-oxidant rich foods
How to detect Colorectal cancer?
There are 4 main testing methods:
Visual testing
Xray and CT testing
Stool “fecal” DNA based testing
Stool blood testing
Colon screening is a critical tool to look for blood, damaged DNA, polyps or cancer
Visual testing: Colonoscopy or Flexible Sigmoidoscopy
A colonoscopy is considered the gold standard of testing. This exam requires a fast and bowel prep the night before the test. During the exam, one is given sedation, and a flexible lighted tube is inserted into your anus and guided through your rectum and colon to look for any signs of cancer or polyps. If found, polyps are removed to biopsy.
Gas is instilled into your colon for this procedure for better visualization, however it may be a challenge to pass gas after the exam. There is a risk of perforation of the colon. When I looked into getting you statistics it was difficult because it was variable, which I am assuming because it depends on the facility and training of the provider. I recommend asking the doctor's personal perforation rates if they have it.
Frequency
Testing is done every 10 years unless you are at high risk for cancer or if polyps are found, then testing is usually recommended every 3 years.
Cost
Most often covered as a “preventative treatment” with insurance. If no insurance, typical cost (GI of Rockies and BCH quotes) is $1900 with conscious sedation and $2100 with anesthesia.
Flexible Sigmoidoscopy
Not commonly recommended because if you are going for an invasive procedure, you should do a Colonoscopy.
Xray and CT Imaging (Computed Tomography “CT” Colonography or "Virtual Colonoscopy")
This screening uses both Xray and CT imaging. You drink contrast solution and air is pumped through a tube into the rectum to expand the area for visualization and images are taken. You will get a report of not only the colon but other important organs in the abdominal area as well, which is a major bonus! This does requires a bowel prep like the colonoscopy, but it requires no sedation. You can have residual bloating and cramping due to the air placement. There is a small risk of puncturing the colon (less than Colonoscopy) and you have small radiation exposure. If any polyps are visualized, you then need a Colonoscopy for removal. Testing: every 5 years Cost: Insurance coverage is variable and less than other screening methods. Cash price on average: $350

Stool-based DNA testing "at home": Cologuard
This test is a Stool DNA, multi-targeted test that looks for certain abnormal sections of DNA from cancer or polyps cells and hidden blood in stool. This DNA stool-based testing is appealing because it can be done at home and there is no bowel preparation or dietary /medication/supplementation restrictions to follow. Unfortunately, if this test is abnormal, you then need a Colonoscopy. This test is not recommended if you are at a high risk for CRD, which includes; personal history of CRC, family history of CRC, IBS, Crohn’s Disease or Ulcerative Colitis. Cologuard is the only test currently in the U.S. that looks for both DNA changes and blood in the stool. Cologuard is a great screening tool for asymptomatic persons at average risk for Colorectal cancer and advanced adenomas (AA). Cologuard can detect 92% of CRC but only 42% of large precancerous polyps. False positives and false negatives do occur. In a clinical study, 13% of patients without Colorectal cancer or advanced adenomas received a positive result (false positive) and 8% of patients with cancer received a negative result (false negative). The clinical validation study was conducted in patients 50 years of age and older. Cologuard performance in patients ages 45 to 49 years was estimated by sub-group analysis of near-age groups. Frequency: every 3 years Cost: Insurance coverage. Medicare covers 100% and about 94% of insured patients have no out-of- pocket cost. Cash price is $581
Stool Based Blood Testing (Fecal Immunochemical Testing and Occult Blood Testing) Fecal Immunochemical Test “FIT”
This home test uses a specific antibody to detect human hemoglobin to detect blood in the stool that wouldn’t normally be visualized in your stool.
Why blood testing?
Blood vessels at the surface of larger polyps or cancers are often fragile and easily damaged by passing stool. These damaged blood vessels usually release a small amount of blood into the stool, but rarely enough to visualize in the stool.
No dietary or supplementary restrictions or prep before testing
You swab stool and place a smear on a card
It's best to do this test 2 days in a row
This test cannot tell if the blood is coming from the colon or other parts of digestive track, such as stomach or hemorrhoids and is less accurate than the Cologuard and visual testing methods. Frequency: Once per year Cost: Fairly inexpensive and covered by most insurances. Pricing appears to be variable $49 to $89 at Quest Direct.
Fecal occult blood test (gFOBT)
Similar test to FIT testing, but this instead uses a chemical guaiac to detect blood in the stool that normally wouldn’t be detected by the naked eye.
Dietary Restrictions before testing are required
You swab stool and place a smear on a card, then let it dry and return it to your clinician’s office or a designated lab to be processed.
Best to do this test 3 days in a row. (I have these at the office)
Frequency: Once per year Cost: Inexpensive. Pricing depends on your provider or the designated testing location “The sensitivity for detecting colorectal cancer was 92.3% with Cologuard and 73.8% with FIT Cologuard, a stool test combining altered human DNA and fecal hemoglobin, showed higher single-application sensitivity than a commercial FIT for both colorectal cancer and advanced precancerous lesions” (see study below) Unfortunately Cologuard has a higher false positive rate than FIT, especialy as people age, possibly leading to a higher rate of unnecessary follow up testing and concern." Colonoscopy is considered the gold standard for finding polyps, precancerous lesions and tumors and removing them during the exam. If polyp or cancer is suspected on all other testing, you then need a Colonoscopy to remove them.
Which tests is right for you?
This depends on your risk factors, your insurance and personal cost, your access, and your personal preference.
How can one prevent colorectal cancer?
Lower your inflammation!
Reducing body fat ‘especially belly fat” is critical
Get moving!!
Stop Smoking
Reduce your toxic load by eating an Organic, GMO free diet
Get those bowels moving. If you have constipation you must work to increase elimination to at least one daily, but ideally 2-3 per day
Increase water intake
Take essential fatty acids as Omega 3's
Work on any emotional layers of "stagnation" that may be negatively affecting the energetic flow to your gut and pelvis. Holding anger and resentment with an inability to forgive perpetuates a low vibration frequency and is a risk factor. Also, if you tend to "over-care "for others and ignore yourself, this will also create stagnation and increase your risk of disease. We are energetic beings after all!
Does eating meat increase risk?
High amounts of red and processed meat can increase heme iron, which is linked to oxidative stress and cellular damage. Processed meats have high nitrates and they contribute to the production of N-nitroso compounds, which damage the lining of the gut (so get nitrate free). Most animal meat is fed with antibiotic feed which damages our microbiome. Grass-fed meat is not fed with antibiotics. However, meat does have good nutrients such as iron, carnitine and B vitamins, which are more difficult to get from plant based diets alone.
Solution? If you are eating meat, make sure it is Grass-Fed, nitrate free and that you have 8-12 servings of phytonutrients per day too!
Always balance your proteins with fiber to protect your microbiome.
PLEASE avoid charring meats! This process releases polycyclic aromatic hydrocarbons and heterocyclic amines, which are known carcinogens (also in cooked and smoked foods). You can marinate in acidic solution and spices and add some rosemary on those special “grill out barbecue days”, to help mitigate those negative effects.
Lowering inflammation also starts with the gut! You need good microbiome support because feeding the good bacteria in your gut is critical to preventing CRC.
Fiber Fiber Fiber! Yes I am bringing this up again because I can’t discuss the importance of this enough to all of you, and to myself. A low fiber diet is a significant risk factor in colorectal cancer!

How high fiber diet can lower risk of colorectal cancer and other factors that increase risk of polyps?
Fiber causes a more dense, heavier stool
Improves immune system
Pulls toxins out of the gut so the carcinogens don’t stick around in the colon causing damage to the cells leading to cancer
Butyrate, a Short Chain Fatty Acid (SCFA) that our gut makes heals the lining of the epithelium (gut lining), so cancer is less likely to grow
Butyrate turns on the tumor suppressor gene
Using fiber to stimulate our endogenous Butyrate production, which is key for fuel for the intestinal track
At BIH we can order an advanced stool test in case you are curious what your Butyrate and microbiome looks like!
Reducing your risk through diet and lifestyle
Eat high fiber foods; nuts, seeds, flax, chia seeds, legumes, beans, whole grains, resistant starches (potatoes and green plantains)
Green leafy vegetables
Avoid fast and processed foods that are high in starches and refined sugars
Diet free of refined sugars and added sweeteners
Limit alcohol to a max of 1 glass of organic red wine for women and 2 glasses for men
Organic, GMO free diet
Eat a variety of foods in the color of the rainbow (see previous blog)
Eat foods high in carotenoids, selenium and lycopenes found in plants
Orange fruits and veggies (for the beta carotene)
Tomatoes, watermelons and pink grapefruit for Lycopene
Brazil nuts for selenium
Almonds and safflower oils, as they are high in Vitamin E
Phytonutrients and Polyphenols from plants to feed the good bacteria
Use more spices for their phytonutrient support
Eat Pomegranates
Curcumin “Turmeric” will change tumor suppressor genes on epigenetic level, which is so cool!
Eat more cruciferous veggies, especially for the Sulforaphane components since they are key to reducing all cancers (or take as a supplement such as Crucera by Thorne)

A Study on drinking tea found that in women specifically, it may reduce risks on an epigenetic levels (green tea has high polyphenols)
Coffee may have positive benefits to prevent cancer (not loaded with sugar or creamers however)
Taking Supplements as Nutrients
You can take Butyrate (depends on brand and type however and again I always only recommend professional brands to know there is regulation on quality and contaminants of the supplements).
Pre and Probiotic supplements (broad spectrum unless you have SIBO, then Soil Based are best).
Melatonin
Antioxidants nutrients such as Selenium, Vitamin A, C, D and E (can’t take Vitamin A if you are a smoker).
Glutathione (master antioxidant and detoxifier in the body) and key to taking with alcohol consumption.
Methylation support helps with dealing with DNA synthesis and DNA damage repair, which is key in preventing cancer, such as: Folate (B9) but not folic acid (especially if you have a MTHFR mutation), Vitamin B6, Vitamin B2, B12 and Glycine (make sure all B's are methylated!).


May you all have a healthy colon and cancer free life! Yours in health and longevity, Carrie Ballas Resources https://aacrjournals.org/cebp/article/28/9/1469/71947/Adherence-to-the-World-Cancer-Research-Fund Adherence to the World Cancer Research Fund/American Institute for Cancer Research 2018 Recommendations for Cancer Prevention and Risk of Colorectal Cancer https://www.cancer.gov/news-events/cancer-currents-blog/2020/colorectal-cancer-rising-younger-adults#:~:text=Rising%20Rates%20around%20the%20World,than%201%25%20of%20younger%20adults. Why is Colorectal Cancer Rising Rapidly among Young adults? https://pubmed.ncbi.nlm.nih.gov/24645800/ Multitarget Stool DNA Testing for colorectal cancer screening https://www.sciencedaily.com/releases/2005/07/050726074406.htm Virtual Colonoscopy Reveals Disease Outside the Colon, As Well https://www.cologuard.com/ https://pubmed.ncbi.nlm.nih.gov/31451044/ Fecal DNA Testing for Colorectal Cancer Screening https://pubmed.ncbi.nlm.nih.gov/24693890/ Adenoma detection rate and risk of colorectal cancer and death https://www.gastrojournal.org/article/S0016-5085(18)30022-2/fulltext Colonoscopy risks: what is known and What Are the Next Steps? https://questdirect.questdiagnostics.com/products/FIT-Colorectal-Cancer-Screening/d41c67cb-a16d-4ad6-82b9-1a77d32daf41 Quest Direct ordering https://academic.oup.com/hmg/article/26/16/3221/3848993?login=false Tea and coffee consumption in relation to DNA methylation in four European cohorts https://www.bmj.com/content/359/bmj.j5024 Coffee consumption and health: umbrella review of meta-analysis of multiple health out comes https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4409470/ Nutrients, Foods and Colorectal Cancer Prevention https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2776517 Role of Diet in Colorectal Cancer Incidence: Umbrella Review of Meta-analyses of Prospective Observational Studies https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6766109/#:~:text=Melatonin%20could%20also%20block%20the,progression%20%5B74%2C%2075%5D. Melatonin https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421942/#:~:text=Methylation%20within%20the%20promoter%20regions,diverse%20number%20of%20human%20cancers. DNA Methylation: An Alternative Pathway to Cancer